Clinical case of a nursing patient with head trauma and elbow dislocation
Characterized by loss of consciousness for less than 5 minutes and histological injury.
On the Glasgow Coma Scale, a mild (TEC) is between 14 or 15. Having these concepts clear, we see that a luxus fracture and mild (TEC) have their different types, causes, symptoms, risk factors, consequences and complications.
It also has its respective diagnosis and treatment of which we will develop in the following work. In the clinical case that we present below, this is a man who suffered a mild (ECT) and a luxus fracture of the left elbow, where the diagnoses and nursing care that we have applied are developed, according to the subjective data and the objective data that we can observe and value in it, when performing the physical examination.
Cranial brain trauma (ECT) has been a health problem since the appearance of man that seriously threatens the patient's life since the head and its contents are compromised: the brain. TEC is an anatomical or functional injury to the scalp, skull, meninges, or brain caused by blunt force.
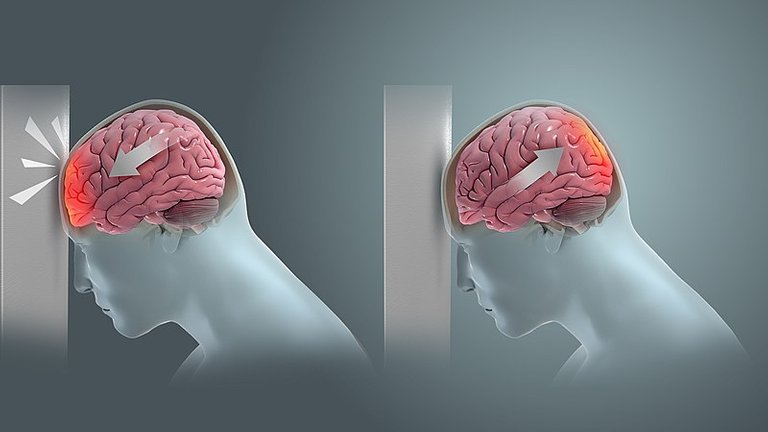
When the traumatic impact occurs, a vibratory shock of varying amplitude occurs and, as a consequence, cerebral edema and displacement of the soft tissues against the hard structures of the skull occur, displacing cerebrospinal fluid, venous blood to a limit imposed by the skull in what is it's called intracranial hypertension.
At the neuron level, depolarization, electrolyte disturbances, cellular metabolism, vascular paralysis and hemorrhages of various degrees occur. As a consequence of these factors, consciousness is compromised, clinically showing the following stages:
- Lucido: The patient is alert, oriented in space and person time.
- Hazy: He tends to fall asleep, but wakes up alone, when he wakes up he is confused with temporary and / or spatial disorientation, lack of notion of danger; may be accompanied by delirium, ideation disorder, and elementary mathematical calculations.
- Sopor: Its natural state is sleep, it wakes up in front of stimuli of different intensity (verbal = superficial drowsiness, pain = deep drowsiness) with periods of psycho-motor arousal: where great psychic and useless motor activity is observed
- Eat: Total unconsciousness resistant to external stimuli, absolute inability to wake up.
The states of consciousness are recovered without a pre-established time, any alteration in the order indicates a complication, which must be investigated.
Classification:
According to the meningeal indemnity they are classified into:
1.Open TEC: lesion with continuity solution of the meningeal sheaths.
2.TEC closed: injury without communication of the brain with the outside.
They are also classified according to their severity:
Mild ECT - Glasgow Scale 14 or 15. Characterized by loss of consciousness for less than 5 minutes and histological injury: brain swelling.
Moderate ECT - Glasgow Scale 9 to 13; characterized by loss of consciousness greater than 5 minutes and histological injury: brain swelling and edema.
Severe ECT Glasgow scale of 3 to 8 characterized by loss of consciousness or coma for more than 30 minutes and histological injury: brain swelling, edema and liquefaction.
Diagnosis:
The level of consciousness is the main prognostic factor in ECT. For its evaluation, the Glasgow coma scale was used, which evaluates 3 clinical parameters: ocular opening, verbal response and motor response. Depending on the degree of commitment in each category, a total score is assigned. Said score ranges from 3 points (maximum commitment) to 15 points (minimum commitment).
Paraclinical diagnosis:
It is indicated that all T.E.C. Mild be studied with emergency cranioencephalic computed tomography (T.A.C.). The T.A.C. It allows evidence of bone and intracranial injuries. If T.A.C. is not available, it is advisable to perform plain skull x-rays (forehead and profile). These radiographs will reveal fracture bone lesions, and eventually intracranial air. Plain skull radiographs do not substitute or provide the same data as the T.A.C.
Their normality does not exclude the possibility of serious traumatic intracranial injuries (bruises, contusions, etc.) and they are not enough to decide behaviors.
Treatment of mild ECT:
If there is a normal level of consciousness (G.C.S. 15), no traumatic pathology is evident in T.A.C. and there are no complications (epileptic seizures, L.C.R. fistulas, otorrhachia, or others) the treatment is only symptomatic.
The use of anticomycials, osmotic diuretics, antibiotics, or other “prophylactic use” drugs is not indicated.
Patients with Glasgow 15 with loss of consciousness, post traumatic amnesia, associated with vomiting, are requested to have a CT scan of the brain and observation for 12-24 hours.
Patients with Glasgow 14: they require a cerebral CT and observation for 24 hours.
Pathophysiology
A mild ECT is one that the Glasgow Scale 14 or 15. characterized by loss of consciousness for less than 5 minutes and histological injury: brain swelling. As we already know, the main cause of mild traumatic brain injury is blows to the head, this can be due to falls in any circumstance, collisions and traffic accidents, fights and domestic violence, sports injuries, explosions or combat injuries and also, Mild traumatic brain injury may also result from a penetrating head injury; This means that any object that enters through the skull or in the brain can cause an injury with characteristics similar to the previous ones. Symptoms of this injury could be headache, confusion, dizziness, vertigo, blurred vision, ringing in the ears, tiredness or drowsiness, bad taste in the mouth, change in sleeping habits, changes in behavior or state of mood, difficulty with memory, concentration, attention or thought, loss of consciousness lasting a few seconds or minutes, sensitivity to light or sound, nausea or vomiting. As there are some causes for mild ECT, a series of age groups have also been determined that represent a risk factor when it comes to suffering a brain injury, these are children between 0 and 4 years old, young adults between 15 and 24 years and adults over 60 years. In any of the previous age groups, the sex of the person also plays a special role, since there is a higher incidence of traumatic brain injury in men than in women. One of the first consequences of traumatic brain injury is loss of consciousness. After the progressive recovery of the level of consciousness and orientation, the majority of patients present a great diversity of physical, cognitive and behavioral sequelae that vary in nature and severity, depending on the extent and location of the brain damage, as well as of personality characteristics.
For this reason, the most relevant cognitive disorders that appear most often are problems of behavior regulation and control, difficulties in abstraction and problem solving, learning and memory disorders, as well as alterations in the field of personality and emotional adjustment. Physical disorders include motor (mobility, language) and / or sensory (vision, hearing, touch and taste) disorders. Finally, Mild ECT Complications could be Subdural Hematoma that are generally due to rupture of the communicating veins between the cerebral cortex and the dura. They are located preferentially in the frontoparietal convexity, their incidence is higher in ethyl patients, the elderly and those with anticoagulant treatment. Acute subdural hematoma requires urgent surgery and they have a high mortality. Traumatic subarachnoid hemorrhage is often accompanied by a concomitant subdural hematoma or a brain contusion. It does not require urgent surgical treatment. And intraparenchymal hematoma, which is where traumatic intraparenchymal hematomas can manifest as rapidly expanding lesions or be asymptomatic. In most cases, there is a cranial fracture associated with a blow or kickback.
Now we will develop a little about the dislocation of the elbow so we will start with the fractures.
Fracture
It is an injury in which the bone is broken or fragmented. In other words, a fracture is the loss of the normal continuity solution of the bone tissue, produced as a consequence of trauma or a debilitating pathological process of its normal structure.
Classification:
- Complete fracture: The bone breaks into two parts.
- Green stem fracture: The bone breaks, but does not separate into two parts. It is typical of children.
- Simple fracture: The bone breaks on the one hand.
- Comminuted fracture: The bone breaks in more than one part or splinters.
- Open fracture: The bone protrudes through the skin.
- Closed fracture: There is a break, but the bone does not protrude through the skin.
Dislocation
It is a separation of two bones in the place where they meet, that is, in the joint. the concept of dislocation refers to an injury that involves the removal of a bone. This dislocation assumes that the bone structure loses contact with the articular surfaces.
Classification
- Simple (not associated with fractures).
- Complex (associated with fractures).
Luxo fracture
As we already know that the term fracture refers to the breakage of a bone and the dislocation refers to the out of place of a bone.
Keeping these terms clear, we can conclude by saying that a luxo fracture occurs when after a bone fracture, if the energy continues to increase this fracture produces displacement and generates a separation beyond normal, producing what is called a luxo fracture.
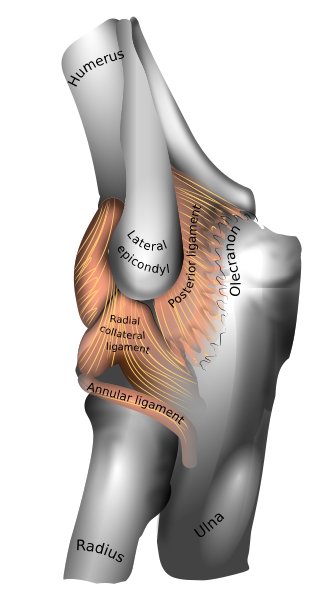
Luxo fractured elbow
After a fracture-associated elbow dislocation, joint instability is generated, so surgical treatment should be the treatment of choice to ensure a good result. Elbow dislocations are second in frequency and are often associated with fractures ( up to 20%) that complicate their treatment and results
Luxo fractures of the elbow generally occur following one of the following injury patterns:
- Posterior dislocation with fracture of the radial head: occurs in up to 5% to 10% of cases.
- Posterior dislocation with coronoid fracture: it also occurs in up to 5% to 10% of cases, secondary to avulsion by the brachial muscle.
- Posterior dislocation with fracture of the radial head, fracture of the coronoid process and tear of the lateral collateral ligament complex. This injury is known as the "terrible triad."
- Injury with varus posteromedial rotational instability associated with fracture of the antero medial aspect of the coronoid process.
- Luxo anterior or posterior fracture of the olecranon.
- Associated fracture of the medial or lateral epicondyle (12% to 34%): it can produce a mechanical block after closed reduction due to entrapment of the fragment.
Luxo anterior fracture of the olecranon
- It is the result of direct trauma to the flexed elbow.
- Some authors suggest that this injury may be caused by the same mechanism that usually causes elbow dislocation, especially in the elderly with osteopenia.
Diagnosis
- The patient typically holds the injured limb, which presents a variable degree of instability and increased volume.
- It is essential to carry out a thorough neurovascular evaluation, which must be carried out before obtaining imaging tests and any manipulation.
- After manipulating or reducing the lesion, the evaluation should be repeated to assess the neurovascular situation.
- Serial neurovascular examinations are necessary when there is a large inflammation in the ante-ulnar region or if it is considered that the patient is at risk of developing a compartment syndrome.
- Angiography may be necessary to assess vascular compromise.
- After reduction, if arterial flow is not restored and the hand continues with poor perfusion, the patient should be prepared for arterial reconstruction with saphenous vein grafting.
- When there is vascular compromise, angiography should be performed in the ward to avoid delaying the operation.
- The radial pulse may be present even if there is an injury to the brachial artery, thanks to the collateral circulation.
- The absence of a radial pulse in a hot and perfused limb probably implies the existence of an arterial spasm.
- Associated fractures generally affect the head of the radius and / or the coronoid process of the ulna.
- Acute neurovascular injuries are rare; The most frequently affected structures are the ulnar nerve and the anterior interosseous branch of the median nerve.
- The brachial artery can be injured, especially in open dislocations.
Imaging evaluation - Standard anteroposterior and lateral radiographs of the elbow should be obtained.
- X-rays must be reviewed to rule out an associated fracture around the elbow.
- CT is useful to identify bone fragments that cannot be seen on plain radiographs.
Treatment of complex elbow dislocation
Non-surgical treatment:
- It is a reasonable treatment option when there is only one dislocation associated with an undisplaced or minimally displaced radial head fracture.
- Patients who opt for non-surgical treatment should be informed of possible instability and that there may be a limitation of mobility or osteoarthritis resulting from fracture of the radial head.
- It is reasonable to remove the splint and start active mobility, under strict supervision, at the first consultation, generally one week after the injury.
Surgical treatment
- Includes repair or replacement of the radial head and repair of the lateral collateral ligament.
- Most of the authors do not recommend the reconstruction of the medial collateral ligament in the acute phase.
- Some authors, however, emphasize the importance of the lateral collateral ligament in the stability of the elbow and are in favor of reinserting it into the lateral epicondyle.
- When the lateral collateral ligament is repaired, it is generally possible to immediately initiate active mobility (especially if capital-radial contact has also been restored), but it is reasonable to immobilize the joint for up to 10 days.
Pathophysiology
A luxus fracture occurs when after a bone fracture, if the energy continues to increase this fracture produces displacement and generates a separation beyond normal, producing what is called a luxo fracture. Some causes that can lead to a dislocated elbow fracture can be traumatic incidents, such as sports injuries, vehicle accidents and falls, health conditions such as osteoporosis, and some types of cancer that make bones break more easily.
In these cases minor trauma and falls can be severe. The symptoms that usually occur in this pathology are usually visibly out of place limb or joint or deformity, swelling, bruising or bleeding, severe pain, numbness and tingling, breakdown of the skin with the protruding bone, limited movement or inability to move a limb and inflammation. There are also risk factors among which we can see the person's age, inheritance and sports. Among the complications that can occur we have blood loss, delayed bone growth that is shown in children since they are in the development stage, nerve puncture, trapped arteries and may increase the risk of osteoarthritis in the future.
Rating
Login data:
Identification:
Name and Surname: W Antonio P G
Provenance: Barinas, Obispo municipality, Los Guasimitos Barinas parish
Service: traumatology.
Room 420, bed 10
Age: 44 years old
Background
Family
-Maternal line: does not refer
-Paternal line: does not refer
-Personal: does not refer
-Psychosocial habits: coffee
-Immunity: complete
Reason for consultation or admission
Because he had a pole fall approximately 4 meters high, he manifested pain in his left elbow and head, and stated that he had lost consciousness for a few minutes after the fall.
Subjective data
Functional patterns
1.Health management-perception pattern:
The patient manifested having had a stable and good state of health throughout his life (I do not state that he has had illnesses or any other type of injury that has caused him to be in poor health until now), therefore, he is considered a healthy person. Currently, emergency admission due to the fall of a pole, approximately 3 meters high, and diagnosis of a TEC level and a luxury invoice left. No surgical intervention has been carried out at the moment, due to lack of materials. The patient has never smoked, consumed alcohol or any other type of drugs. He has all of his shots and has no known allergies at the moment.
2. Nutritional-metabolic pattern:
The patient is referred to a complete diet and his diet is balanced since he refers to eating the 3 respective meals of the day. Drink plenty of fluids and have a good appetite. He has full teeth, with a normal swallow, and his bowel sounds are within normal DLN limits. It has no skin problems and has good color and hydration of the skin and mucosa. He has a wound on his left elbow, he has no edema and his body temperature is 36.7 ° C.
3.Removal pattern:
Urinate approximately 7 times a day and is painless when urinating. Its urine has good color and appearance. Evacuate twice a day and do not have excessive sweating.
4.Activity-exercise:
Its activity is limited and its weakness diminished due to the fracture of the left elbow. All her self-care of daily life is dependent, since she needs help to do them. T.A: 132/75 mmHg. F.C: 63 bpm, F.R: 19 rpm.
5. Sleep-rest pattern:
The patient reports not resting properly because he is in an environment with 6 other people and is awakened by noise and also because he is concerned about his family, since he is the main caretaker of his home.
6. Connective-perceptual:
It does not present any alteration of its senses (auditory, visual, olfactory, gustatory and tactile).
7. Self-perception-self-concept:
The patient feels useless in the hospital, and wants to return home as soon as possible since he is the primary caregiver for his family.
8. Role-relationships:
He lives with his wife and 2 children, and receives support from his wife.
9. Sexuality-reproduction:
It has no sexual or reproductive problems. He currently has 2 children who are alive.
10. Coping and stress tolerance:
Since the fall that the patient presented, he manifests concern for his family since he is the main caregiver and the one who works for their support. Being in the hospital makes him feel useless and he already wants to go home.
11. Values-beliefs pattern:
The patient is an evangelical Christian, attends a church, and believes in a supreme being.
Vital signs:
Blood Pressure: 132/75 mmHg
Heart Rate: 63 bpm
Pulse: 61 ppm
Respiratory Rate: 19 rpm
Temperature: 36.7 ° C
Physical exam:
This is a 44-year-old male patient, a native of the town of Barinas and from the Obispo Municipality, Los Guasimitos Parish, sector August 28; who was admitted to the DR Luis Rapetti hospital due to an obstetric emergency because he suffered a post fall and presented pain in the upper left limb and in the head. He was diagnosed with mild ECT and a dislocated left elbow fracture. He is currently on the 3rd floor in the trauma area, room 420-10, awaiting surgery. On physical examination; neurological: conscious, oriented in its 3 planes (time, space and person). Respiratory: FR: 19 rpm, normal expandable symmetrical chest without pain points, audible vesicular murmurs in both lung fields; no respiratory distress tolerating ambient O2. Cardiovascular: present and audible heart sounds without aggregates. HR: 63 bpm, TA: 132/75 mmHg, with a palpable and regular pulse of 61 ppm. Capillary filling for 1 sec, without presentation of edema. Nutritional and metabolic: flat and soft abdomen without pain points, with air-borne noises present, tolerating a complete diet. It presents good swallowing, it has complete teeth and a good appetite, it refers to evacuate 3 times a day without any difficulty. Genito / urinario: genitalia of appearance and normal configuration according to age and sex. He refers to urinate 7 times a day without pain when urinating, he has no edema and his urine output is normal in color and appearance. Integumentary: brown skin, hydrated and normotemic with a temperature of 36.7 ° C. With permeable route in the right upper limb.
Nursing diagnoses:
1): RC sleep pattern disorder: responsibilities as caregiver and noises CSDP: verbal complaints of not feeling well rested
2): Impairment of physical mobility RC: intolerance to activity and deterioration of physical state CSDP: limitation of range of motion.
3): Impaired mobility in RC bed: musculoskeletal impairment
CSDP: impaired ability to change position by oneself in bed
4): Risk of disuse syndrome RC: mechanical immobilization 5): Fatigue RC: anxiety CSDP: inability to maintain normal activities
6): Risk of intolerance to CSDP activity: deterioration of physical condition
7): Self-care deficit: RC feeding: musculoskeletal impairment CSDP: inability to bring food from a container to the mouth, open the containers, and pick up the cup or glass.
This post has been voted on by the SteemSTEM curation team and voting trail. It is elligible for support from @curie and @minnowbooster.
If you appreciate the work we are doing, then consider supporting our witness @stem.witness. Additional witness support to the curie witness would be appreciated as well.
For additional information please join us on the SteemSTEM discord and to get to know the rest of the community!
Thanks for having used the steemstem.io app and included @steemstem in the list of beneficiaries of this post. This granted you a stronger support from SteemSTEM.